Underserved communities like Gary-Lake Station face challenges in diabetes management and weight loss due to limited access to fresh produce and healthcare. Telehealth Ozempic consultations offer a solution by providing virtual guidance from home, breaking geographical barriers. This approach builds community support systems for Ozempic users, addressing food desert issues and fostering healthier lifestyles. By integrating telemedicine into obesity care, healthcare professionals can enhance adherence, improve health outcomes, and empower residents in these communities.
In underserved areas like Gary-Lake Station, where healthcare access is limited, Ozempic—a groundbreaking diabetes treatment—offers hope. However, successfully integrating self-care routines among its users poses unique challenges. This article explores strategies to enhance their well-being. We delve into the impact of Ozempic on these communities, highlighting the transformative potential of telehealth ozempic consultations in Gary-Lake Station. Additionally, we discuss innovative solutions like addressing food deserts with telemedicine-based obesity care and building community support systems for Ozempic users, fostering sustainable health improvements.
- Understanding the Impact of Ozempic on Underserved Communities
- Telehealth Consultations: Revolutionizing Diabetes Management in Gary-Lake Station
- Addressing Food Deserts: A Digital Solution for Sustainable Obesity Care
- Building Community Support: Empowering Ozempic Users Through Connection
- Strategies for Effective Self-Care Routines: Nurturing Well-being from Within
Understanding the Impact of Ozempic on Underserved Communities

In underserved communities, like Gary-Lake Station, access to quality healthcare and obesity management resources is often limited, creating a unique challenge for residents relying on Ozempic® (semaglutide) injections for diabetes treatment and weight loss. These areas, frequently characterized by food deserts—places with limited or no access to fresh, affordable produce—present specific barriers to maintaining healthy routines. Integrating telehealth into the care landscape offers a promising solution, providing Ozempic consultations via virtual platforms, which is particularly beneficial for individuals who may face transportation hurdles or have busy schedules.
By leveraging telemedicine-based obesity care, healthcare professionals can extend their reach into these communities, offering guidance and support tailored to local needs. This approach not only addresses the immediate medical requirements of Ozempic users but also has the potential to foster community support systems. Encouraging peer-to-peer connection among Ozempic users in underserved areas can create a network of individuals who understand the unique challenges they face, ultimately enhancing adherence to self-care routines and promoting healthier lifestyles.
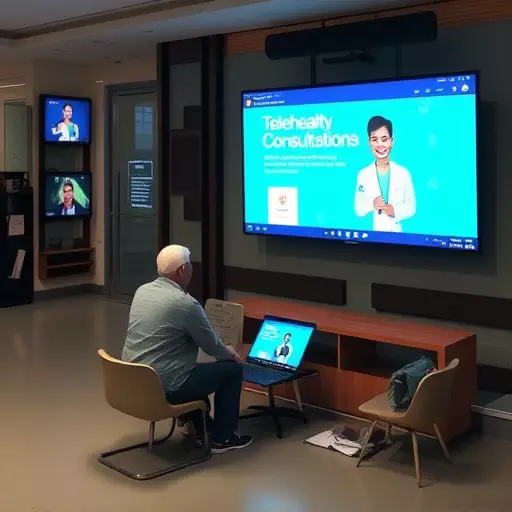
Telehealth Consultations: Revolutionizing Diabetes Management in Gary-Lake Station

In Gary-Lake Station, a community grappling with limited access to healthcare and often referred to as a “food desert,” telehealth consultations are transforming diabetes management for Ozempic users. This innovative approach allows patients to receive personalized medical advice and support from the comfort of their homes, breaking down geographical barriers that have historically hindered care. By leveraging telemedicine, healthcare providers can reach underserved populations who might otherwise struggle to access specialized diabetes care, ensuring they stay on track with their self-care routines.
Through virtual consultations, community health workers and nutritionists guide Ozempic users through the intricacies of their treatment plans, offer tailored advice on diet and exercise, and address any concerns or challenges unique to living in a food desert environment. This holistic approach not only improves individual health outcomes but also builds much-needed community support systems. By fostering connections among peers facing similar health journeys, these virtual gatherings create a network of encouragement and shared knowledge, empowering Gary-Lake Station residents to take charge of their diabetes management and embrace healthier lifestyles.
Addressing Food Deserts: A Digital Solution for Sustainable Obesity Care

In underserved areas like Gary-Lake Station, addressing food deserts is a critical step towards sustainable obesity care. Many communities facing food insecurity rely on limited and often unhealthy food options, exacerbating health disparities. Telehealth ozempic consultations offer a promising solution by connecting patients directly with healthcare providers for personalized guidance on medication management, diet, and exercise. This digital approach overcomes geographical barriers, ensuring that individuals in remote areas can access expert care without the need to travel long distances.
Building community support systems for Ozempic users within these communities is equally vital. By leveraging telemedicine, healthcare providers can facilitate group consultations, creating a sense of belonging and encouraging peer-to-peer learning. This collaborative environment fosters better adherence to self-care routines, ultimately contributing to improved health outcomes. Such initiatives not only promote individual wellness but also strengthen the overall resilience of underserved communities.
Building Community Support: Empowering Ozempic Users Through Connection

In underserved communities like Gary-Lake Station, addressing healthcare disparities is essential, especially when it comes to managing chronic conditions like type 2 diabetes. Telehealth ozempic consultations offer a revolutionary approach to providing specialized care. By utilizing telemedicine, patients can connect with healthcare professionals remotely, ensuring accessible and convenient treatment options, even in areas considered food deserts. This innovative strategy not only overcomes geographical barriers but also fosters a sense of community support for Ozempic users.
Building community support systems is crucial in empowering individuals to maintain self-care routines. Through online forums, support groups, or local community initiatives, Ozempic users can find like-minded individuals who understand their challenges and celebrate their successes. These connections encourage adherence to treatment plans, provide emotional support, and offer practical advice on navigating daily life with a chronic condition. Addressing food deserts with telemedicine-based obesity care is a step towards creating inclusive healthcare solutions that truly make a difference in underserved communities.
Strategies for Effective Self-Care Routines: Nurturing Well-being from Within

In underserved areas like Gary-Lake Station, where addressing food deserts with telemedicine-based obesity care is paramount, promoting self-care routines for Ozempic users goes beyond individual efforts. Building community support systems becomes a powerful strategy. Telehealth Ozempic consultations can facilitate connection among users, fostering a sense of belonging and accountability. By creating virtual or in-person support groups, individuals can share experiences, offer encouragement, and exchange practical tips on managing diabetes and maintaining healthy habits.
This collective approach nurtures well-being from within, empowering users to stick to their self-care routines. Regular check-ins with healthcare professionals via telehealth can further ensure that any concerns or challenges are promptly addressed. Combining these initiatives strengthens the community’s overall health and resilience, making it easier for Ozempic users in underserved areas to thrive.