Rural communities like Evansville-Henderson, KY-IN face challenges in accessing and utilizing Semaglutide for diabetes management due to regional laws, limited healthcare resources, and cultural considerations. These obstacles manifest in delayed prescriptions, inadequate provider training, and a lack of tailored patient education. To bridge this gap, targeted initiatives involving local networks, community organizations, and policymakers are crucial to enhance Semaglutide availability, improve provider knowledge, and foster culturally sensitive healthcare delivery, ensuring better diabetes management for diverse populations.
In the global landscape of healthcare, Semaglutide has emerged as a game-changer in diabetes management. This article delves into the trends and challenges surrounding Semaglutide’s accessibility within rural healthcare systems, using Evansville-Henderson, KY, as a case study. We explore regional laws and their impact on prescriptions, analyzing diverse legal frameworks and their effects on patient outcomes. Additionally, cultural considerations are examined, highlighting strategies for culturally sensitive care in low-resource, rural settings, particularly when integrating traditional practices with modern Semaglutide therapy.
- Semaglutide Availability and Access in Rural Communities: A Case Study of Evansville-Henderson, KY
- – Exploring the local landscape of diabetes management
- – Challenges faced by rural healthcare providers in prescribing Semaglutide
Semaglutide Availability and Access in Rural Communities: A Case Study of Evansville-Henderson, KY

In rural communities like Evansville-Henderson, KY, the availability and accessibility of Semaglutide—a powerful diabetes medication known for its versatility and efficacy—present unique challenges. Despite its potential to significantly improve glycemic control, regional laws impacting semaglutide prescriptions can create barriers to care. Limited healthcare resources and a shortage of specialized providers in these areas often result in delayed access, affecting patients’ management plans. For instance, Evansville-Henderson’s demographics and cultural considerations play a role in the adoption of semaglutide therapy. Local communities may have diverse cultural backgrounds that influence dietary preferences and lifestyle choices, requiring tailored education and support for successful medication adherence.
These factors underscore the need for targeted initiatives to bridge the gap in semaglutide access. Collaborating with local healthcare networks, community organizations, and policymakers can help ensure that rural residents in Evansville-Henderson and similar areas benefit from advanced diabetes management options like semaglutide. This involves addressing regulatory hurdles, enhancing provider training, and promoting cultural sensitivity in healthcare delivery.
– Exploring the local landscape of diabetes management

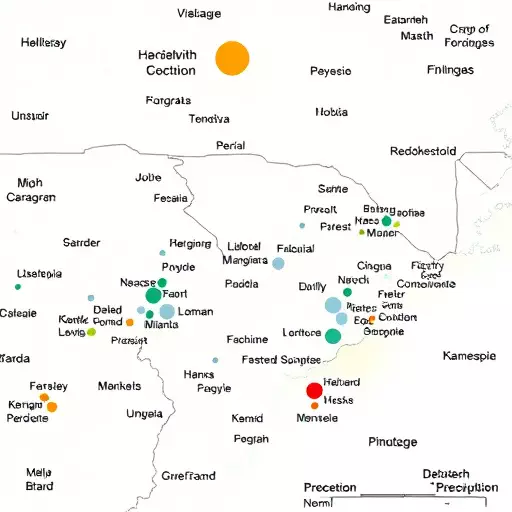
In exploring the local landscape of diabetes management, particularly in areas like Evansville-Henderson, KY-in, one discovers a unique blend of healthcare challenges and opportunities. The availability and prescription patterns of Semaglutide, an innovative medication for type 2 diabetes, vary significantly across regions due to various factors. Regional laws impacting semaglutide prescriptions play a crucial role in shaping access to this game-changing therapy. For instance, different states may have unique regulatory frameworks dictating how healthcare providers can prescribe and manage medications like Semaglutide, influencing both its availability to patients and the training requirements for healthcare professionals.
Cultural considerations also significantly shape the integration of Semaglutide into rural healthcare systems. In a bustling community with diverse cultural backgrounds, such as Evansville-Henderson, understanding local beliefs, preferences, and barriers to care is essential. For example, certain cultural practices or dietary habits may impact how patients engage with semaglutide therapy, requiring tailored educational approaches and support systems. By delving into these aspects, healthcare providers can ensure that Semaglutide is not only accessible but also effectively utilized within the unique fabric of rural communities.
– Challenges faced by rural healthcare providers in prescribing Semaglutide

Rural healthcare providers often face unique challenges when it comes to prescribing Semaglutide, a medication that has shown great promise in managing type 2 diabetes. One significant hurdle is accessibility; rural areas typically have limited pharmaceutical resources and specialized clinics, making it difficult for patients to gain access to this treatment option. This issue is further exacerbated by regional laws and regulations that may differ across states, impacting the availability of Semaglutide and creating inconsistencies in prescription practices. For instance, in Evansville-Henderson, KY-in, healthcare providers must navigate local policies that could restrict or delay patient access to such advanced medications.
Additionally, cultural considerations play a vital role in semaglutide therapy. Rural communities often have diverse ethnic backgrounds and unique cultural practices that may influence patients’ acceptance of new treatments. Healthcare providers need to be sensitive to these factors and adapt their approach accordingly. Effective communication, addressing concerns, and tailoring treatment plans to align with cultural beliefs can significantly enhance patient adherence and outcomes in rural settings.