In Gary-Lake Station, a remote community facing food deserts and high obesity rates, Telehealth Ozempic Consultations provide a game-changing solution. This telemedicine initiative offers accessible, personalized weight loss care, including guidance on Ozempic, an effective type 2 diabetes medication aiding in weight management. By removing physical clinic visits, it tackles transportation barriers and privacy concerns. Furthermore, building community support systems among Ozempic users enhances treatment adherence and fosters successful weight loss journeys. These virtual connections normalize health conversations, combat stigma, and empower residents to collectively work towards healthier environments.
In many communities, particularly remote areas like Gary-Lake Station, access to specialized healthcare, especially for weight loss management, remains limited. This article explores how telehealth Ozempic consultations are transforming care in these regions, offering a gateway to accessible treatment. We delve into the benefits of telemedicine for tackling food deserts and improving nutritional guidance. Additionally, we discuss building robust community support systems for Ozempic users, fostering success and long-term adherence through education, peer groups, and partnerships aimed at enhancing health outcomes.
- Telehealth Ozempic Consultations: A Gateway to Accessible Care in Gary-Lake Station
- – Exploring the benefits of telemedicine for remote communities
- – Success stories and patient experiences with virtual consultations
Telehealth Ozempic Consultations: A Gateway to Accessible Care in Gary-Lake Station
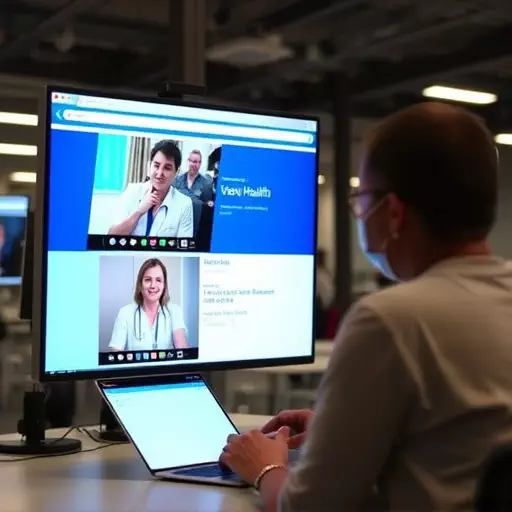
In the heart of Gary-Lake Station, a community facing challenges similar to many other urban areas, including food deserts and obesity rates, Telehealth Ozempic Consultations have emerged as a revolutionary solution. This innovative approach to healthcare delivery leverages telemedicine to make specialized weight loss care more accessible. By offering remote consultations, patients can connect with medical professionals who provide guidance on using medications like Ozempic (semaglutide), a popular injectable drug for type 2 diabetes that has shown promising results in weight management.
Addressing food deserts with telemedicine-based obesity care allows individuals to receive personalized advice and support without physically visiting a clinic. This is especially beneficial for those who face barriers such as limited transportation, busy schedules, or concerns about privacy. Building community support systems for Ozempic users further enhances the effectiveness of these consultations. By fostering connections among patients, they can share experiences, offer encouragement, and create a network that promotes adherence to treatment plans, ultimately contributing to more successful weight loss journeys.
– Exploring the benefits of telemedicine for remote communities

In remote communities like Gary-Lake Station, where addressing food deserts is a pressing issue, telemedicine offers a promising solution for providing obesity care. Through telehealth Ozempic consultations, individuals can access specialized weight loss management from the comfort of their homes, overcoming geographical barriers and ensuring consistent support. This innovative approach is especially beneficial for those living in areas with limited healthcare access, enabling them to receive personalized guidance on medication use, diet plans, and lifestyle changes.
Building community support systems for Ozempic users through telemedicine enhances the overall effectiveness of weight loss programs. By facilitating virtual connections between residents, healthcare providers, and nutritionists, these platforms foster a sense of camaraderie and shared purpose. This network can help combat the stigma associated with weight loss medications by normalizing conversations around health and providing a safe space for individuals to share their experiences and successes. Moreover, community-based telemedicine initiatives empower members to take charge of their well-being and collectively work towards creating healthier environments.
– Success stories and patient experiences with virtual consultations

Many patients have successfully navigated their weight loss journeys with the help of virtual telehealth consultations, particularly in areas like Gary-Lake Station where addressing food deserts with telemedicine-based obesity care is becoming increasingly popular. These sessions allow individuals to connect with healthcare professionals from the comfort of their homes, removing geographical barriers and making specialized care more accessible. The use of technology in this context has proven beneficial for various reasons.
One notable advantage is the ability to share experiences and build community support systems for Ozempic users. Through virtual platforms, patients can interact with peers facing similar challenges, fostering a sense of belonging and encouragement. Success stories shared within these communities inspire others, demonstrating that weight loss medications like Ozempic can be effectively integrated into sustainable lifestyle changes. This exchange of experiences is invaluable in reducing the stigma often associated with seeking medical assistance for obesity, especially when coupled with personalized care tailored to individual needs.
